British Geriatric Society Meeting 2024
12 July 2024
The National Poisons Information Service (NPIS) Cardiff unit successfully submitted an abstract poster to the British Geriatric Society Spring Meeting 2024. The abstract was titled “Using poisons centre data to identify potential safety risks associated with the use of monitored dosage systems.”
This was a collaboration between the UK NPIS, Swansea Bay University Health Board and AWTTC following discussion with members from each organisation after meeting at the AWTTC Best Practice Day 2023.
Abstract:
Introduction: Monitored dosage systems (MDS) encompass a wide range of devices to help management of medication. This research uses poison centre data to explore risks associated with their use.
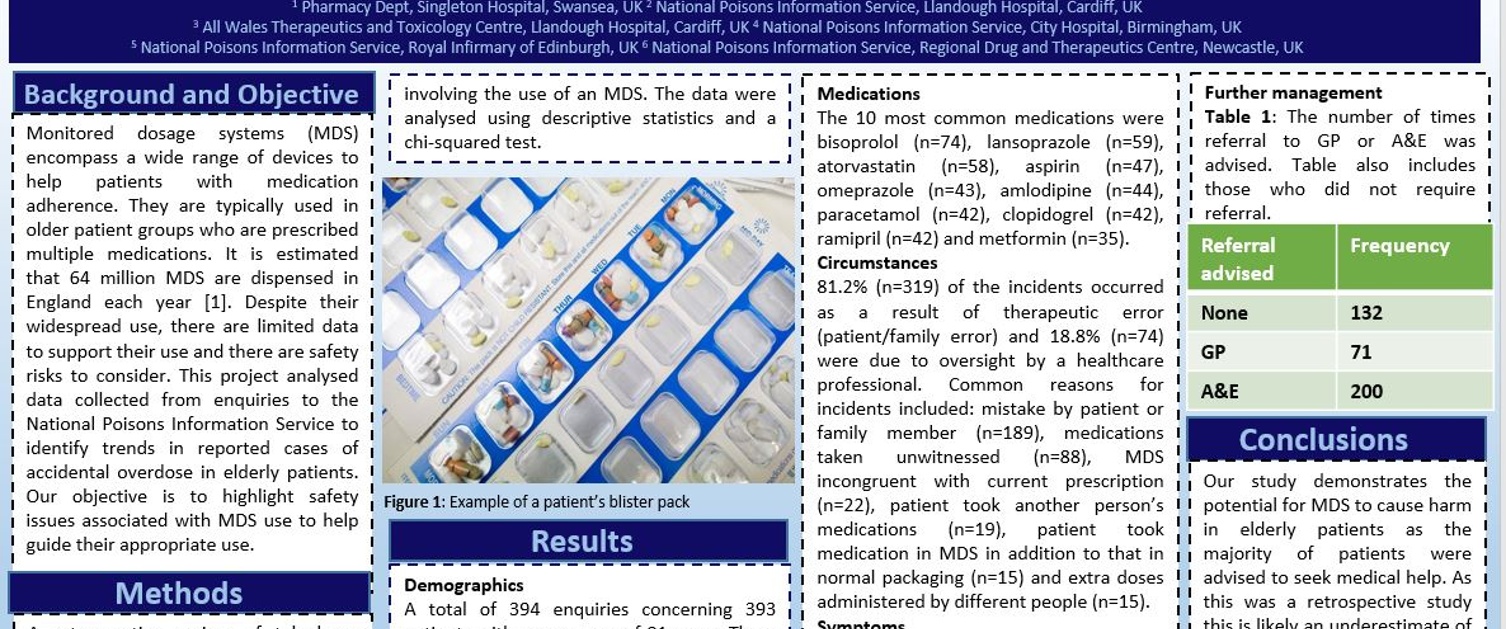
Method: A search of accidental overdose enquiries to the UK National Poisons Information Service (NPIS) between 1/01/2017-31/12/22, classified as “therapeutic error/medical error” involving patients aged 65 or over was performed. Enquiries involving an MDS were identified. Data were analysed using descriptive statistics and chi-square test.
Results: There were 394 enquiries concerning 393 patients and mean patient age was 81 years. There were significantly more females(n=266) than males(n=127), p = <0.0001. Exposures occurred at home (n=372), in care homes(n=18), in prisons(n=2) and in hospital(n=1). Cognitive impairment was reported in 32.5% patients(n=127). The 10 most common medications involved were bisoprolol (n=74), lansoprazole(n=59), atorvastatin(n=58), aspirin(n=47), omeprazole(n=43), amlodipine (n=44), paracetamol(n=42), clopidogrel(n=42), ramipril(n=42) and metformin(n=35). Most patients were asymptomatic(n=312). Common symptoms recorded were somnolence(n=16), dizziness (n=13), confusion(n=11), fatigue(n=7) and hypotension(n=5). Common reasons for incidents were a mistake by patient or family member(n=189), medications taken unwitnessed(n=88), MDS incongruent with current prescription(n=22), patient took another person’s medications(n=19), patient took medication in MDS in addition to that in normal packaging (n=15) and extra doses administered by different people(n=15). Almost 51% of patients were recommended to attend Emergency Department (ED) by the NPIS(n=200) and 18% were advised to contact their GP(n=71).
Conclusion: MDS are perceived to improve adherence, these results reveal their potential harm. For example, most of patients in these enquiries were advised to seek medical help. MDS harm is likely underreported as this was a retrospective study and some information was not routinely collected. Further work including a prospective study is needed alongside support of safer medicine use through improved communication, education, and alternative tailored support.
The poster was well received by conference attendees and is an example of the importance of collaboration between different organisations to combine data and knowledge to inform and improve existing processes.
This abstract is being developed into a research paper and will hopefully be submitted to the BGS journal Age and Ageing this year.
Link to BGS Spring Meeting 2024 website here.